The Different Types of Diabetes, Defined
Source: UNC Health Talk.
More than 30 million Americans have diabetes, but there are many misconceptions about what it does to the body, who can get it and how it’s treated. We talked to UNC Health Care experts to create this explainer.
The Disease
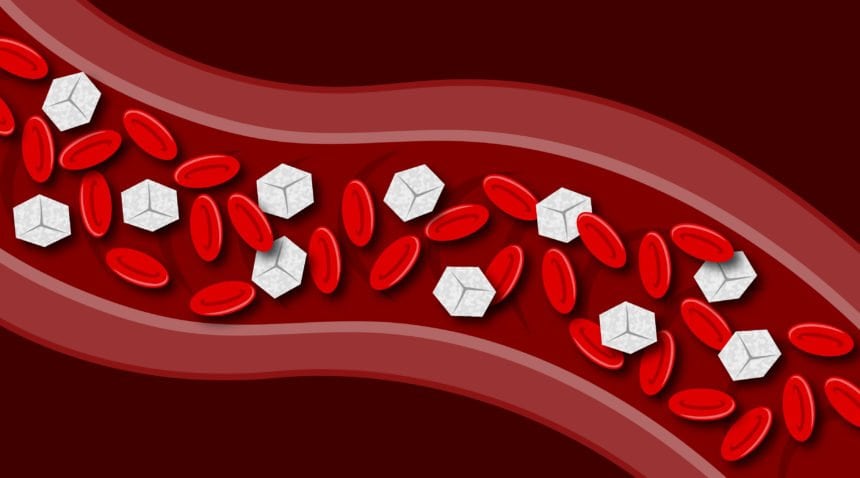
“Diabetes in all its forms is essentially excess sugar in the bloodstream,” says Deepa Kirk, MD, medical director of the UNC Hospitals Diabetes and Endocrinology Clinic at Meadowmont and associate professor of medicine in the UNC School of Medicine.
Sugar, specifically glucose, is the main source of energy for the cells in our body. Glucose from the carbohydrates we eat gets broken down by our digestive system and passed into our bloodstream, which we can think of as the energy delivery highway. Blood carries glucose throughout the body, delivering it to cells that absorb the nutrient.
“Cells are unable to absorb glucose without the hormone insulin, which is produced by beta cells in the pancreas,” Dr. Kirk says. “When that insulin is hampered in some way and glucose isn’t adequately absorbed by cells, glucose stays in the bloodstream causing high blood glucose, or hyperglycemia.”
Blood sugar can be measured through a variety of blood tests. High blood sugar has a number of effects on the body, including low energy and fatigue. If your cells aren’t getting the energy they need, they don’t perform at 100 percent, meaning you don’t feel 100 percent.
“Too much glucose in the bloodstream for too long can also hurt the blood vessels carrying that glucose,” Dr. Kirk says.
Higher than normal blood glucose levels cause blood vessels to contract more, allowing less blood to pass throughout the body. Poor blood flow can cause microvascular and macrovascular damage. Micro damage affects small blood vessels that supply blood to organs. The eyes, kidney and nerves are typically harmed by micro damage. Macro damage affects large blood vessels that supply blood to the heart, brain and limbs. Stroke, heart attack and amputation can result from macro damage.
The most common types of diabetes are type 1, type 2 and gestational. While the general effects of diabetes on the body are the same, the causes and management of high blood glucose vary among the different types of the disease.
Type 1 Diabetes
What causes it: An autoimmune response where the body’s defense system mistakenly attacks the beta cells in the pancreas that produce insulin, resulting in very little or no insulin being produced. Symptoms tend to appear quickly because of the drastic change in blood glucose levels.
Symptoms include: Increased thirst, frequent urination, bed-wetting in children who previously didn’t wet the bed, unintended weight loss, fatigue and blurred vision.
Who can get it: Anyone, no matter their weight, age or ethnicity. It used to be called juvenile-onset diabetes because the symptoms usually start when people are children or young adults, however diagnosis can happen at any age. Those with a family history of type 1 diabetes have a slightly higher chance of getting it and should be screened.
How common is it: About 1.25 million Americans have type 1 diabetes.
How is it managed: Regular insulin injections every day for people with type 1 diabetes are crucial. Without them, a patient could die. Patients have to continuously monitor their blood glucose levels and give themselves doses of insulin when needed. There are multiple options for patients to keep track of their blood glucose levels and deliver insulin injections. An insulin pump is a catheter placed under the skin that allows the patient to deliver insulin with more flexibility.
Can it go away: At this time, type 1 diabetes is considered a chronic disease that lasts a lifetime. More research needs to be done on what actually causes the autoimmune response that attacks the insulin-producing cells. In the most extreme cases, a pancreas transplant can potentially cure diabetes, though the side effects are significant.
Type 2 Diabetes
What causes it: Insulin resistance (the body doesn’t respond to insulin the way it should) and relative insulin deficiency (the body is making insulin, but not enough to counteract insulin resistance).
Symptoms include: The same as for type 1, along with slow-healing sores, frequent infections and areas of darkened skin—usually in the armpits and neck.
Who can get it: Type 2 diabetes used to be called adult-onset diabetes because it is commonly diagnosed in adults, but it can happen at any age. The exact causes are unknown but thought to be a combination of genetic and environmental factors. It can remain undetected for many years until it’s found during a screening or when high amounts of blood glucose start to cause complications. This is why routine screenings are important for those at higher risk for type 2 diabetes: people with a family history, people who are not Caucasian, people who smoke, people who are overweight or sedentary, people over the age of 45, women who have had gestational diabetes, and a child they carried during such a pregnancy.
The very early stages of type 2 diabetes are called prediabetes, which means the body’s blood glucose levels are higher than normal but not high enough to be diagnosed as diabetes. Those with prediabetes could develop type 2 diabetes over time.
How common is it: It’s the most common type of diabetes among the 30 million Americans with diabetes, accounting for 90 to 95 percent of all cases.
How is it managed: Type 2 also is also referred to as noninsulin-dependent diabetes, because unlike for patients with type 1 diabetes, insulin injections are not necessarily a required part of daily life. Type 2 can be managed with a combination of healthy diet, increased exercise, weight loss, medications and insulin injections if needed.
Can it go away: Yes. Some patients, with weight loss and lifestyle changes, can reverse type 2 diabetes, but that outcome is rare. Many patients can control it with diet and exercise at first but eventually need a combination of oral medications and insulin injections. That doesn’t mean that weight loss still can’t have significant effects; even modest degrees of weight loss and dietary changes can make a dramatic difference in diabetes control.
Gestational Diabetes
What causes it: Pregnancy. Something about pregnancy itself makes all pregnant women more resistant to insulin when they reach around 20 weeks gestation. More research is needed to understand exactly why this happens.
Symptoms include: Most women do not have symptoms, but if they do appear, they are similar to those for types 1 and 2 diabetes: increased thirst, frequent urination, fatigue and nausea.
Who can get it: Pregnant women. It is associated with complications to both mother and baby during pregnancy.
How common is it: One in 25 pregnancies worldwide result in the development of gestational diabetes. All women with adequate access to health care, except those with known cases of diabetes, are screened for gestational diabetes during pregnancy.
How is it managed: Mild cases can be managed through diet and physical activity. Other cases require insulin injections. When managed well, pregnancies with gestational diabetes most often result in delivery of a healthy baby.
Can it go away: Yes. Gestational diabetes usually goes away within days or weeks after delivery. But women who develop gestational diabetes and the child they carried during that pregnancy are at a higher risk of developing type 2 diabetes later in life. About half of women with gestational diabetes develop type 2 diabetes five to 10 years after pregnancy.
Other Types of Diabetes
There are other, much less common types of diabetes. These include secondary diabetes, which is a rise in glucose caused by medications, such as those used for organ transplants or steroids. Damage to beta cells that occurs during pancreatitis can affect insulin production and cause diabetes. Specific gene mutations can also affect insulin production, but these cases are often misdiagnosed as type 1 diabetes. All of these types of diabetes are managed with insulin injections or a combination of injections and oral medications.
Common Misconceptions about Diabetes
Michelle Mielke, RD, LDN, is a certified diabetes educator for patients at the UNC Hospitals Diabetes and Endocrinology Clinic at Meadowmont. She says there are many misconceptions about diabetes. Some of them include:
You can’t eat carbs anymore: While patients with diabetes need to be aware of how many carbohydrates they are consuming, a diagnosis of diabetes doesn’t mean you have to cut them out of your diet completely. A balanced, healthy diet of fruits, vegetables, lean protein and complex carbohydrates is advised for most everyone, including people living with diabetes.
People only get type 2 because they’re overweight: Being overweight or obese is a contributing factor to type 2 diabetes and can make blood glucose levels more difficult to control. It is rarely the only reason for type 2 diabetes.
High blood glucose levels are all a person with diabetes needs to worry about: Patients with diabetes can also experience low blood glucose levels (hypoglycemia) if they take too much insulin, or if they do not eat enough or exercise more than anticipated when taking insulin or several other diabetes medications. If not addressed quickly, low blood glucose levels can cause someone to faint, have a seizure or go into a coma. Mielke teaches patients what to do if their blood glucose goes below 70 mg/dl. She says to quickly eat or drink 15 grams of easily digestible sugar such as three to four glucose tablets, a half cup of juice or soda, three to four hard candies, or one tablespoon of sugar.
Are you concerned about diabetes? Talk to your doctor about having your blood glucose levels tested. Learn about diabetes services offered by Johnston Health or call our Diabetes Hotline at 919-209-3386 to speak to one of our Certified Diabetes Educators.